Introduction
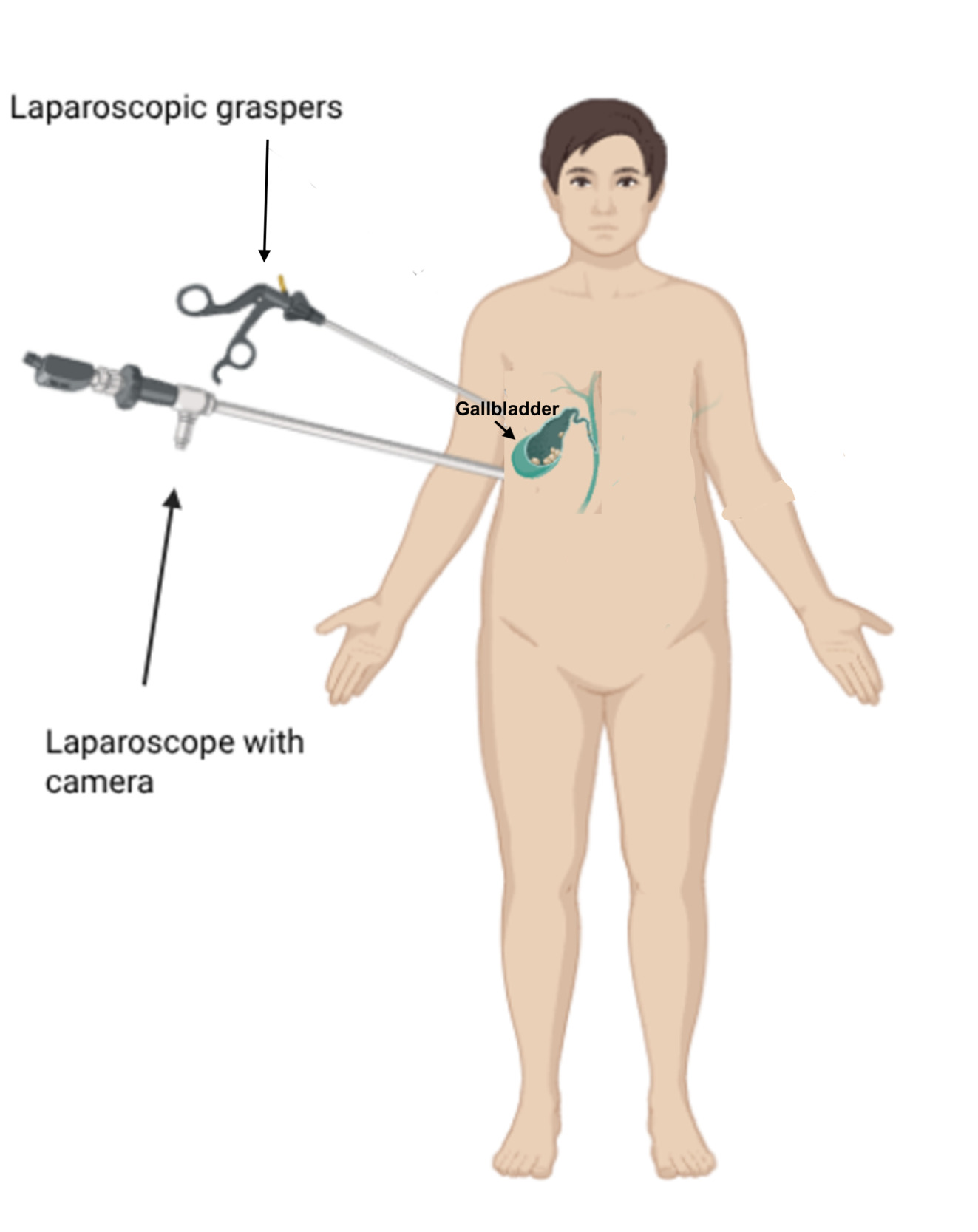
Laparoscopic cholecystectomy (LC) is one of the most frequently performed surgical procedures in the United States and is widely regarded as a safe, minimally invasive intervention for the treatment of symptomatic cholelithiasis and cholecystitis.1,2 The laparoscopic approach uses small incisions, a camera, and specialized instruments to remove the gallbladder [Figure 1], typically resulting in reduced postoperative pain, shorter hospital stays, and faster recovery compared to open surgery.1 Despite its favorable safety profile, LC is not without risk. A subset of patients experiences serious postoperative pulmonary complications, including pneumonia, unplanned intubation, and ventilator dependence, all of which are associated with increased morbidity, prolonged hospitalization, higher resource utilization, and, in some cases, death.3
Previous literature has largely focused on complications such as bile duct injury,4,5 bleeding, or infection following LC, with less emphasis on respiratory outcomes.6 However, pulmonary complications remain clinically significant, particularly in older or medically complex patients. Understanding which patients are at greatest risk for these adverse outcomes is essential for improving preoperative counseling, optimizing perioperative management, and targeting quality improvement initiatives.3
The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) provides a unique opportunity to explore these outcomes on a national scale. As a prospectively collected, risk-adjusted database encompassing over 200 perioperative variables and 30-day outcomes, the NSQIP enables robust, generalizable analysis of postoperative complications.7 In this study, we use the NSQIP database to identify clinical predictors of pneumonia, unplanned intubation, and ventilator dependence within 30 days of LC, with the goal of informing risk stratification and guiding preventive strategies in routine surgical practice.
Pneumonia is an infection in the lungs that can occur postoperatively, which is significant because it can delay the healing of a patient after their procedure.8 The clinical manifestations of pneumonia include a compromised egophony test, dullness to percussion, an increased temperature (typically above 100℉), and other abnormal vital signs.9 Postoperative pneumonia is typically treated with antibiotics and the use of respiratory support.10
Intubation is the process by which an external aid is provided to maintain or secure a patient’s airway, typically by inserting a tube into the trachea to ensure adequate ventilation and oxygenation.11 This is done as part of general anesthesia; but when a patient needs to be re-intubated after extubation, this is an unplanned intubation, and it is usually emergent.12
Ventilation is the circulation and exchange of gases in the lungs, which results in the expulsion of carbon dioxide. Mechanical ventilation is used to both ventilate and oxygenate patients who cannot breathe effectively. When patients become ventilator dependent, it means that they cannot breathe on their own without an endotracheal tube connected via a circuit to a mechanical ventilator.13 Most patients who undergo general anesthesia are extubated and off the ventilator within 48 hours post-operation. Ventilator dependence beyond 48 after surgery is thus considered a complication.
Methods
Data Source
Data were obtained from the NSQIP Participant Use File (PUF) for 2018–2022.14,15 The database includes standardized data collection by trained reviewers and captures over 200 perioperative variables, including patient demographics, comorbidities, laboratory values, intraoperative details, and 30-day outcomes.16 All data were de-identified. As a retrospective quality improvement project, this study received a non-Human Subject determination by Brown University.
Study Design, Patient Population, and Variable Definitions
Inclusion criteria consisted of patients between 18 and 90 years old who underwent LC between 2018–2022. Exclusion criteria consisted of missing or unknown essential variables (e.g., ASA class, functional status, or laboratory data). Predictor (independent) variables: age, sex, BMI, ASA classification, diabetes, smoking status, chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), renal failure, functional status, and white blood cell (WBC) count. Variables were chosen based on prior evidence of clinical relevance. Outcome (dependent) variables included: 1) pneumonia (OUPNEUMO), 2) unplanned intubation (REINTUB), and 3) ventilator dependence >48 hours (FAILWEAN), as coded by NSQIP.14
Statistical Analysis
Descriptive statistics summarized baseline characteristics. Univariate analyses identified factors with p < 0.10. These variables were included in multivariate logistic regression models for each outcome. Odds ratios (ORs) with 95% confidence intervals (CIs) and p-values are reported. Model performance was assessed using area under the receiver operating characteristic curve (AUC).17 Analyses were performed in JMP Pro 17.0 for the Macintosh.
Results
The cohort consisted of 222,537 patients. Table 1 summarizes cohort characteristics.
Pneumonia
Among 222,537 patients, 1011 (0.45%) developed postoperative pneumonia. Elevated preoperative WBC count emerged as the strongest predictor (OR 1.073 per unit, p < 0.0001), followed by higher ASA class (p < 0.0001), advanced age (p < 0.0001), and non-independent functional status (OR 2.54, p < 0.0001). Other significant predictors included steroid use, smoking, COPD, CHF, and renal failure.
Unplanned Intubation
Out of 156,931 patients, 124 (0.08%) required unplanned intubation. ASA class (p < 0.0001) and functional dependence (OR 2.92, p < 0.0001) were the strongest predictors, followed by COPD (p < 0.0001), renal failure (p = 0.0012), older age (p < 0.0001), and elevated WBC (p < 0.0001).
Ventilator Dependence >48 Hours
Of the 156,931 patients, 92 (0.06%) required prolonged mechanical ventilation (>48 hours). Significant predictors included ASA class (p < 0.0001), renal failure (OR 5.29, p < 0.0001), functional dependence (OR 2.78, p < 0.0001), COPD (p = 0.0302), CHF (p = 0.0131), and elevated WBC (p < 0.0001).
Model Performance
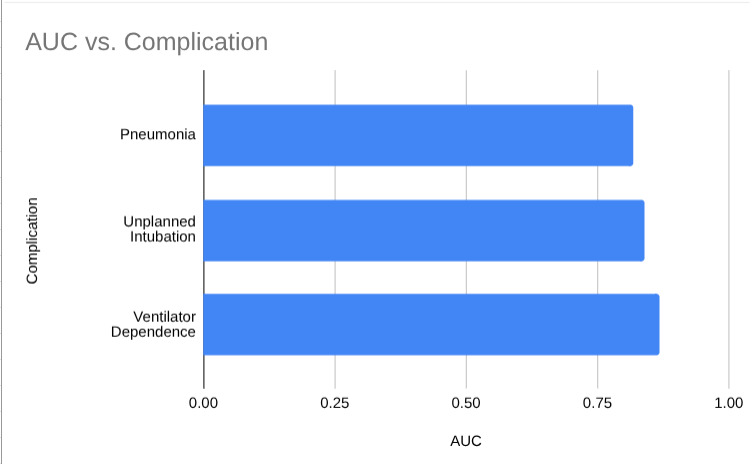
Each logistic regression model demonstrated strong predictive performance, with AUC values of 0.819 (pneumonia), 0.8388 (unplanned intubation), and 0.8674 (ventilator dependence). Figure 2 illustrates these AUC values, emphasizing that the model for ventilator dependence had the highest predictive accuracy, all AUC values are in the same “very good” range.
The incidence of pneumonia was 0.54%, and was significantly associated with elevated WBC, higher ASA class, older age, and functional dependence. The incidence of unplanned intubation was 0.08% and was significantly associated with ASA class, COPD, renal failure, and elevated WBC. The incidence of ventilator dependence beyond 48 hours was 0.06% and was significantly associated with renal failure and ASA class. Across all models, ASA class and functional status were consistent high-risk predictors. The model’s accuracy were strong, with AUC values ranging from 0.819 to 0.867.
Discussion
Our analysis demonstrates that ASA class, functional dependence, elevated WBC count, and comorbidities such as renal failure, COPD, and CHF are robust and consistent predictors of pulmonary complications following laparoscopic cholecystectomy (LC). These findings underscore the critical role of preoperative risk assessment and highlight specific patient factors that warrant closer perioperative management.18
Among the predictors, ASA class emerged as the single strongest risk factor, with ASA class 4 patients experiencing over a 30-fold increase in the odds of unplanned intubation compared to ASA class 1. This dramatic gradient underscores how a patient’s baseline physiological reserve profoundly impacts their ability to tolerate surgery and anesthesia. Functional dependence—a marker of frailty and limited mobility—was also highly predictive, indicating that patients with reduced independence are less likely to recover adequate airway control after anesthesia.19 Renal failure, likely due to its association with systemic inflammation, electrolyte imbalance, and fluid overload, further increased the likelihood of airway compromise. The model’s high accuracy (AUC = 0.8388) suggests these predictors are both reliable and clinically meaningful, making them ideal for preoperative screening and perioperative planning.19
A similar pattern was observed for prolonged ventilator dependence. ASA class and renal failure again dominated as key predictors, with ASA 4 patients exhibiting over a 20-fold increase in risk compared to ASA 1. Elevated WBC counts, indicative of pre-existing infection or systemic inflammation, were also significant, as was older age, which correlates with diminished pulmonary reserve. The model’s AUC of 0.8674, the highest of all three complications, demonstrates that these variables can accurately identify patients who may require extended postoperative respiratory support.18 Clinically, this emphasizes the need for proactive ventilatory planning, including early respiratory therapy and ICU-level monitoring for high-risk patients.20
Pneumonia, while the most frequent complication, presented a more multifactorial risk profile. Elevated WBC count (unit OR 1.073) was the most powerful predictor, emphasizing the importance of identifying preoperative infections or inflammatory states. ASA class, BMI, smoking, and COPD were also strongly associated with pneumonia risk, reflecting the interplay between systemic health and pulmonary defense mechanisms.21 Smoking and COPD, for example, impair mucociliary clearance, increasing susceptibility to lower respiratory infections. The AUC of 0.819 indicates that our model is highly effective at distinguishing patients who are most vulnerable to pneumonia.
Significance and Implications
These results align with and extend findings from previous studies, reaffirming that functional status and systemic inflammation are as important as traditional comorbidities like COPD or CHF when predicting postoperative outcomes.22 From a clinical perspective, this means that interventions such as prehabilitation programs, smoking cessation, and optimization of chronic diseases (e.g., CHF, renal dysfunction) could substantially reduce postoperative pulmonary risks.23 Additionally, identifying patients with elevated ASA scores preoperatively allows for tailored perioperative care, including enhanced airway management, early mobilization, and aggressive pulmonary hygiene measures.24
By combining easily measurable preoperative variables (ASA class, WBC, comorbidities) with functional status, the models presented here offer a practical and data-driven tool for surgical teams to stratify risk, optimize care pathways, and potentially reduce postoperative morbidity. The high AUC values across all models (0.819–0.867) underscore the robustness and clinical utility of these predictors.16
Limitations
This study is limited by the retrospective nature of NSQIP data; for example, ASA class and functional status are subjectively assessed, potentially introducing variability. The analysis includes only U.S. hospitals participating in NSQIP, which may limit generalizability to other populations. Additionally, the study period (2018–2022) excludes earlier or later data.15,17
Conclusion
Our findings indicate that higher ASA class, systemic inflammation (as reflected by elevated WBC counts), functional dependence, and key comorbidities such as COPD, CHF, and renal failure are strong and consistent predictors of postoperative pulmonary complications following laparoscopic cholecystectomy (LC). These variables reflect not only the patient’s underlying physiologic reserve but also the presence of chronic disease and inflammatory states that increase vulnerability to respiratory failure or infection.
Recognizing these risk factors preoperatively allows surgical teams to implement targeted interventions, such as optimizing medical conditions, improving functional capacity through prehabilitation, and planning for advanced respiratory support when needed. For example, patients with high ASA scores or impaired functional status may benefit from aggressive perioperative pulmonary care, early mobilization, and closer ICU monitoring. Similarly, identifying and addressing systemic inflammation prior to surgery may help mitigate the risk of pneumonia or delayed ventilator weaning.
Furthermore, the predictive accuracy of our logistic models (AUC values ranging from 0.819 to 0.867) underscores the reliability of these variables as practical risk stratification tools. Incorporating them into routine preoperative evaluations can improve patient counseling, guide resource allocation, and ultimately enhance postoperative outcomes.