Introduction
Spontaneous coronary artery dissection (SCAD) is an under-diagnosed and under-recognized cause of acute coronary syndrome (ACS), accounting for up to 4% of ACS cases and over 25% of myocardial infarctions (MI) in women under 50 years of age.1 It is characterized by a non-iatrogenic, non-traumatic separation of the coronary arterial wall with false lumen formation, leading to impaired coronary perfusion.2 SCAD typically occurs in individuals without traditional atherosclerotic risk factors and has been associated with fibromuscular dysplasia, connective tissue disorders, pregnancy, systemic inflammatory diseases, and emotional or physical stress.3 Clinical presentation may include features of MI or life-threatening ventricular arrhythmias depending on the degree of blood flow compromise.4
Diagnosing SCAD solely based on angiographic findings is often challenging; therefore, intravascular imaging modalities, such as intravascular ultrasound (IVUS) and optical coherence tomography (OCT), may be used when angiographic results are inconclusive.5 Observational studies suggest that conservative therapy is often preferred for hemodynamically stable patients, as many dissections spontaneously heal over weeks to months. Percutaneous coronary intervention (PCI) may be indicated in cases of ongoing ischemia or life-threatening ventricular arrhythmias, but it carries higher technical complexity and a risk of dissection propagation.6 In this case, we present a case of SCAD in a young woman with acute anterior MI, highlighting the importance of early recognition, imaging-guided diagnosis, and individualized management.
Case Presentation
A 32-year-old woman presented to the emergency department with sudden-onset, severe retrosternal chest pain radiating to the left arm, associated with diaphoresis and nausea. She had no history of hypertension, diabetes mellitus, smoking, or hyperlipidemia. Her obstetric history included one full-term vaginal delivery two years earlier. Family history was negative for premature coronary artery disease.
Upon presentation, her vital signs were as follows: blood pressure 128/78 mmHg, heart rate 92 beats/min, respiratory rate 16 breaths/min, and oxygen saturation 98% on room air. Physical examination was unremarkable.
Initial laboratory evaluation revealed markedly elevated high-sensitivity troponin I at 3.4 ng/mL (reference <0.04 ng/mL), and elevated CK-MB at 45 U/L (reference range 0–25 U/L). Other laboratory parameters, including complete blood count, renal function, and lipid profile, were within normal limits (Table 1).
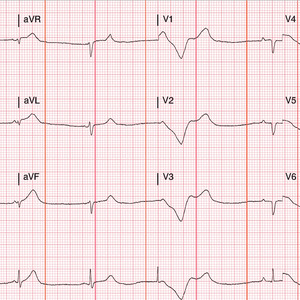
Electrocardiography demonstrated ST-segment elevation in leads V2–V5, consistent with acute anterior myocardial infarction (Figure 1). Transthoracic echocardiography revealed mild hypokinesis of the anterior wall with preserved left ventricular ejection fraction (LVEF 55%) and no valvular abnormalities.
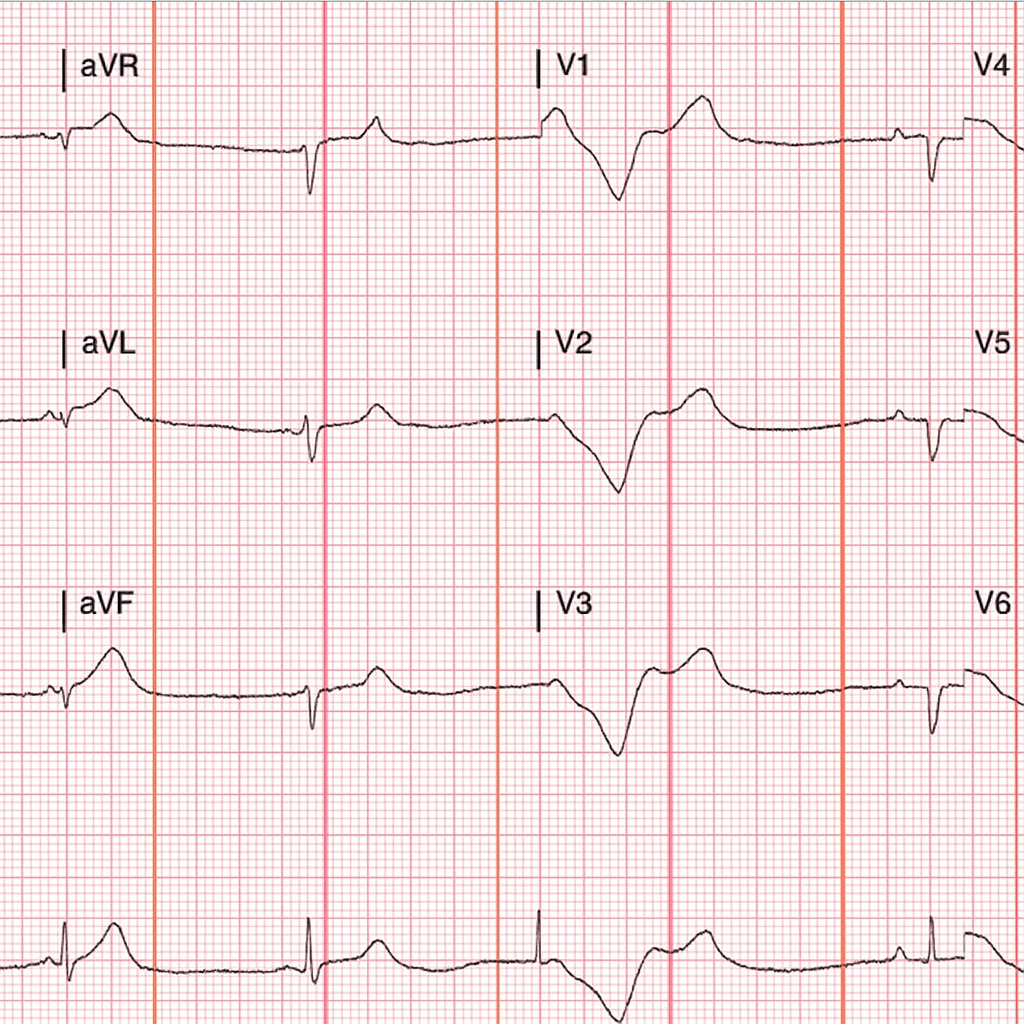
Emergent coronary angiography revealed a long, diffuse narrowing of the mid-left anterior descending (LAD) artery with preserved distal flow (Thrombolysis in Myocardial Infarction [TIMI] grade 3) and no evidence of atherosclerotic plaque or thrombus (Figure 2A). Optical coherence tomography confirmed the presence of an intramural hematoma and intimal flap, establishing the diagnosis of spontaneous coronary artery dissection (SCAD) (Figure 2B). The patient remained hemodynamically stable with no ongoing chest pain.
Given the preserved distal flow and stable hemodynamics, a conservative management strategy was adopted. The patient was initiated on dual antiplatelet therapy with aspirin and clopidogrel, a beta-blocker therapy for heart rate control, and a statin therapy for secondary prevention. She was closely monitored in the cardiac intensive care unit for 48 hours and remained asymptomatic. Serial cardiac biomarkers declined, and ECG changes gradually resolved.
At 3 months, follow-up coronary computed tomography angiography (CCTA) demonstrated partial resolution of the dissection with improved vessel caliber. By 12 months, follow-up imaging revealed complete healing of the LAD artery with restoration of normal vessel architecture (Table 2). Clinically, the patient remained asymptomatic, maintained normal functional status, and experienced no recurrence of ischemic events.
Discussion
Spontaneous coronary artery dissection is now widely recognized as an important cause of myocardial infarctions, accounting for up to one quarter of MIs in women younger than 50 years of age, it also represents a notable etiology of acute coronary syndrome, especially among females without conventional risk factors.7
Pregnancy, the peripartum state and the postpartum period - reported in 2% to 18% of cases, are well-established risk factors for SCAD.8 These conditions may contribute through hormonal changes that weaken the coronary arterial walls in combination with increased hemodynamic stress, SCAD frequently coexists with Fibromuscular dysplasia (FMD), as has been documented in 72% of nonatherosclerotic-SCAD patients included in a study conducted at Vancouver General Hospital.9
Notably, spontaneous coronary artery dissection may also occur in the absence of traditional risk factors as illustrated by our 32-year-old patient. This emphasizes the need to maintain a high index of suspicion, early recognition, and accurate diagnosis, even in otherwise healthy young women. Most importantly, since SCAD can resemble or mimic atherosclerotic myocardial infarction, a misdiagnosis may lead to inappropriate PCI attempts that may worsen the outcome.
Coronary angiography is performed as a first-line diagnostic tool, particularly in the presence of ST-segment elevation. However, certain SCAD lesions, such as those classified as type 3,10 could mimic atherosclerosis with focal or tubular stenosis. Therefore, advanced intravascular imaging techniques such as optical coherence tomography (OCT) and intravascular ultrasound (IVUS) are essential, as diagnosis can be made even with intimal flaps and/or intramural hematoma being present.11 In our case, optical coherence tomography provided definitive evidence of SCAD, guided a conservative strategy, and helped to avoid unnecessary PCI.
In stable patients, a conservative management is generally the preferred approach. Revascularization with PCI or coronary artery bypass grafting (CABG) is preserved for patients with ongoing ischemia, left main dissection, or hemodynamic instability. This recommendation is informed by the angiographic findings that most SCAD lesions typically heal spontaneously, while revascularization carries high failure rates, and does not reduce SCAD recurrence risk.12,13 Our patient demonstrated this course, with OCT confirming arterial healing at 12 months. Medical therapy typically includes beta-blockers to decrease arterial wall stress, in addition to antiplatelet therapy for secondary prevention, as implemented in this case. Regular clinical follow-up combined with serial noninvasive imaging, such as CCTA, is valuable for tracking vessel healing, assessing residual dissections, and providing reassurance of recovery.
The long-term sequelae are generally favorable with conservative treatment. However, recurrence is not uncommon. Most recurrent events occur within the first few years and are more likely in patients with coronary tortuosity or fibromuscular dysplasia (FMD), both of which are associated with higher recurrence risk.14 Therefore, patient counseling, risk factor modification, avoidance of triggers, and structured follow-up are essential.
This case highlights the importance of maintaining a high index of suspicion for SCAD in young women presenting with ACS, irrespective of their risk factor profile, underscores the value of multimodality imaging for accurate diagnosis, and demonstrates the effectiveness of conservative management when appropriate.
Conclusion
Spontaneous coronary artery dissection (SCAD) is a rare but important cause of acute myocardial infarction in young women without traditional cardiovascular risk factors. Early recognition, accurate diagnosis with multimodal imaging, and appropriate conservative management are crucial to optimizing outcomes and minimizing procedural complications. This case highlights the importance of considering SCAD in differential diagnosis for acute coronary syndromes in this population, emphasizes the role of imaging in guiding therapy, and demonstrates that long-term recovery with complete arterial healing is achievable with careful follow-up and multidisciplinary care.
Ethical Considerations
Written informed consent was obtained from the patient for publication of this case report and accompanying images.

.jpg)
.jpg)